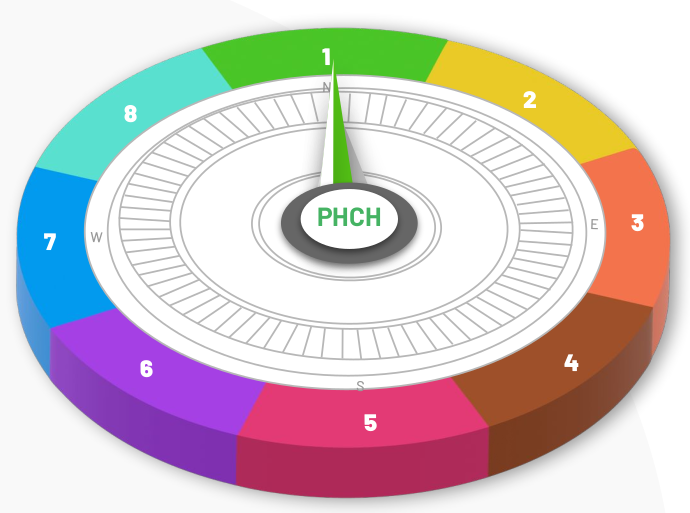
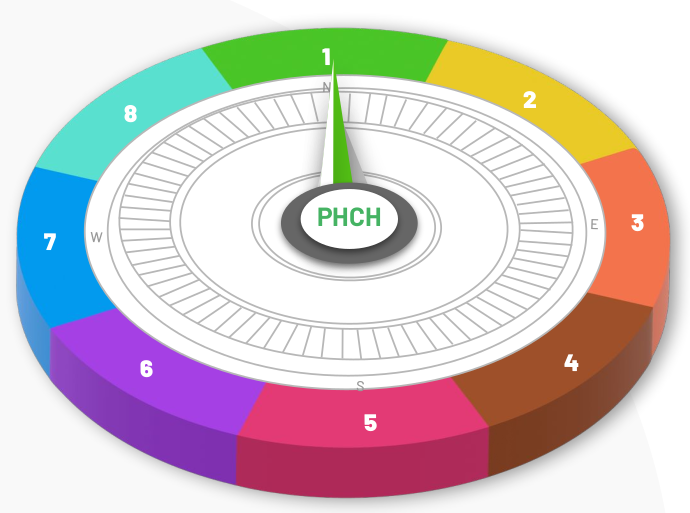
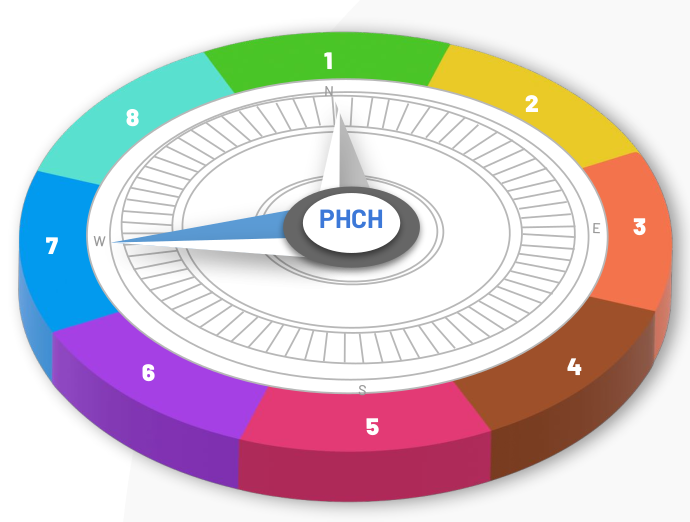
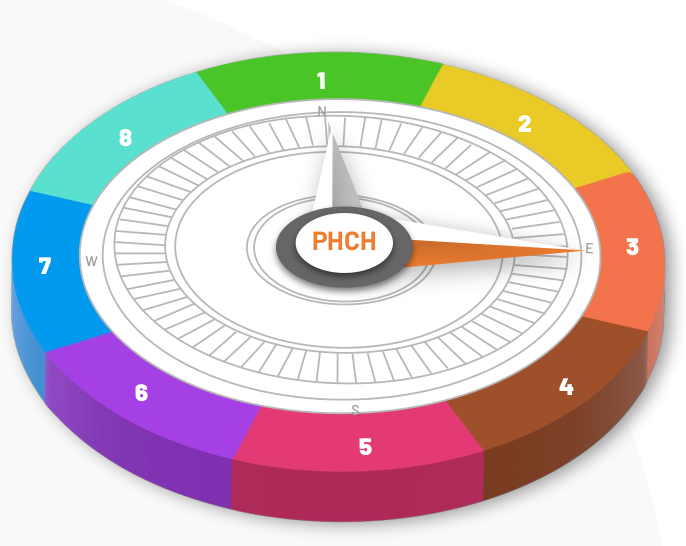
Enhance Clinic Flow
Clinician’s schedules are optimized for high value, using the EMR as a tool
Patient interaction time is optimized through standardized, synchronized resources
Patient schedules are optimized
Environments are optimized
Processes are standardized
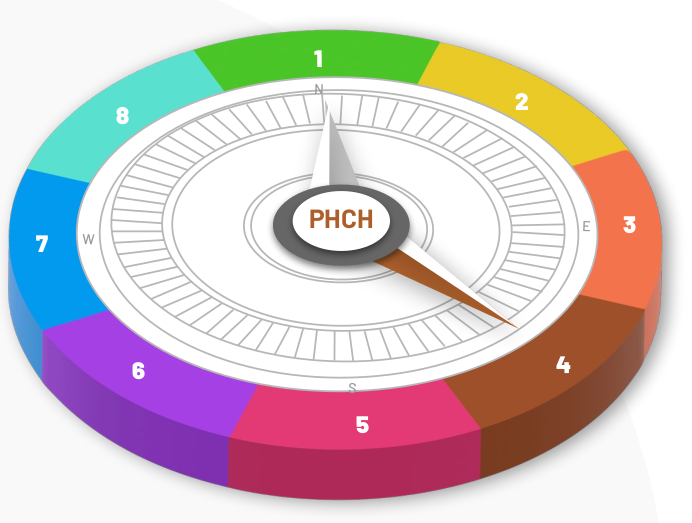
Coordinated Care and Seamless Transition
Clinical care planning is integrated within the care team and specialty transitions are monitored for ease of referral
- Accountability and tracking are improved
- Relationships are developed and strengthened
- Patients are supported
- Connectivity is apparent
- Care coordination agreements are in place
Teams and Teamwork
Primary care providers are supported by a team, with clear roles and common approaches to provide patient-centered wrap-around services based on care needs
- The right condition for team success is set
- Team functions, roles and responsibilities are optimized
- Team coordination and communication is effective
- Cooperation and shared cognition are enhanced
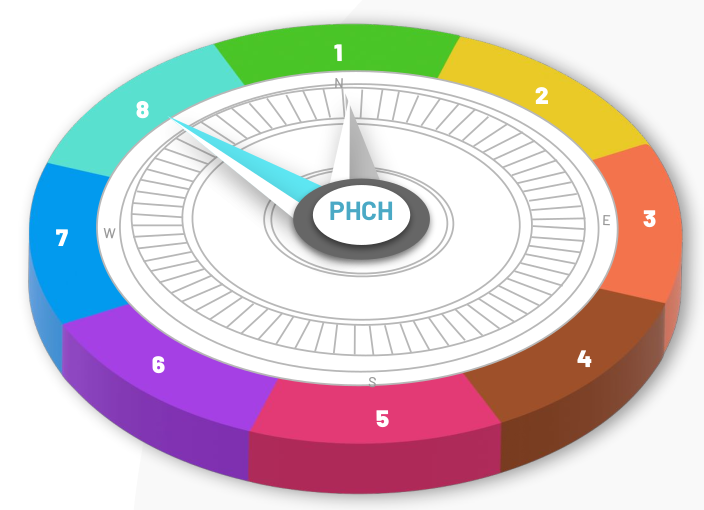
Person-Centered Interactions
Teams respect patient identity and promote shared decision-making to align values and needs.
- Culture, values and gender preferences are respected
- Patients are engaged in decision making
- Self-management supports are maximized
- Impact of patient experiences is recognized
- Patient-centered communication is practiced
- Safety is a primary focus, notwithstanding the patient-provider power imbalance
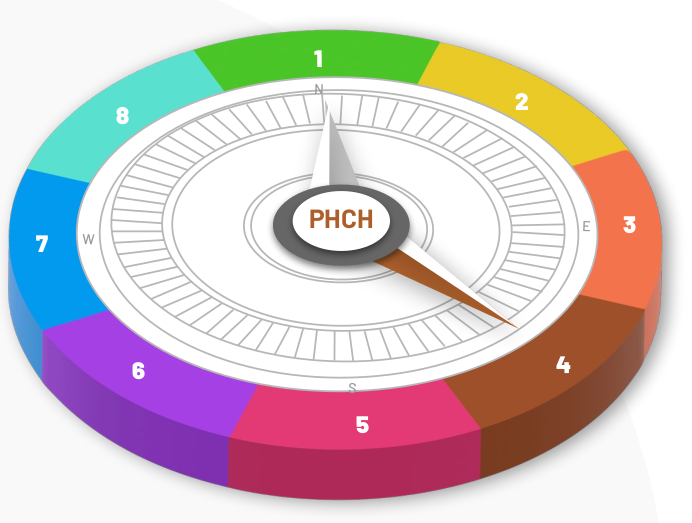
Proactive Panel Management
Needs of patient sub-groups are identified and systematic, pro-active approaches to deliver tailored individual planned patient care are built.
- Patients for Proactive Panel Management are identified
- Care delivery processes are redesigned
- Evidence-based decision supports are integrated
- EMRs are optimized for common clinical workflow
- Care planning processes are activated
- Team work for panel management is optimized
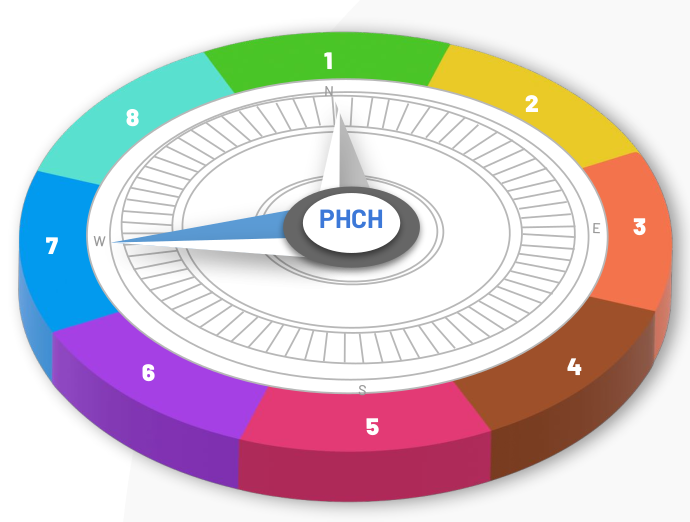
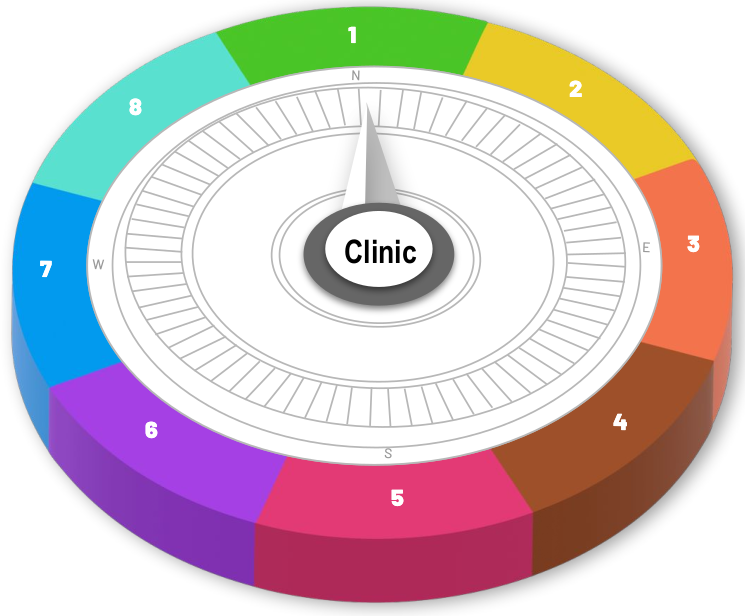
High Impact Changes for Primary Care
Provide Access and Continuity
Processes designed to optimize access to appointments and to increase relational, informational and management continuity are employed.
- Supply and demand are balanced to meet panel needs without waiting
- Supply time is increased to provide care
- Panel demands for appointments are reduced
- Panels are adjusted between most responsible providers, as needed
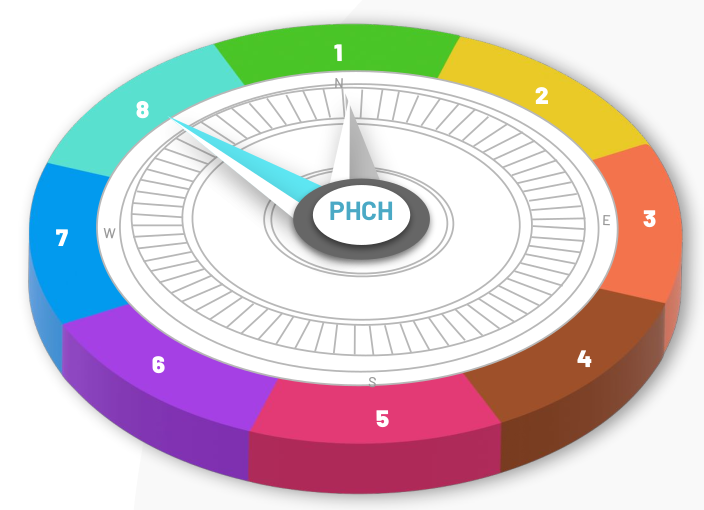
Know Your Patient Panel
Each patient has a dedicated primary care provider (a physician or nurse practitioner) supported by a team familiar with their story. Clinic teams coordinate screening, prevention, management and treatment needs in partnership with the patient.
- Commitments to primary care provider access and continuity are made
- Panel lists are identified and maintained
- Panel workloads are evaluated and understood
- Needs of the panels are assessed
- Patients are engaged in the improvement process
- Teams are optimized to best meet panel needs
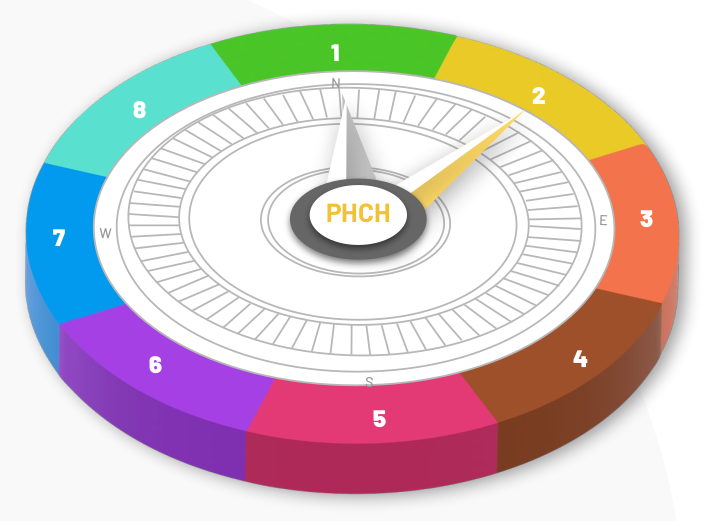
Build a Culture of Quality Improvement
Clinic leaders and team members champion continuous improvements using proven methods.
- Clinic leaders assess and build readiness and will for change
- Quality plans are built based on the Sequence to Achieve Change
- Practice facilitation supports are identified / enhanced
- EMRs are optimized for quality improvement
- Patients are engaged in the improvement process
Clinician’s schedules are optimized for high value, using the EMR as a tool
Patient interaction time is optimized through standardized, synchronized resources
Patient schedules are optimized
Environments are optimized
Processes are standardized
Clinical care planning is integrated within the care team and specialty transitions are monitored for ease of referral
- Accountability and tracking are improved
- Relationships are developed and strengthened
- Patients are supported
- Connectivity is apparent
- Care coordination agreements are in place
Primary care providers are supported by a team, with clear roles and common approaches to provide patient-centered wrap-around services based on care needs
- The right condition for team success is set
- Team functions, roles and responsibilities are optimized
- Team coordination and communication is effective
- Cooperation and shared cognition are enhanced
Teams respect patient identity and promote shared decision-making to align values and needs.
- Culture, values and gender preferences are respected
- Patients are engaged in decision making
- Self-management supports are maximized
- Impact of patient experiences is recognized
- Patient-centered communication is practiced
- Safety is a primary focus, notwithstanding the patient-provider power imbalance
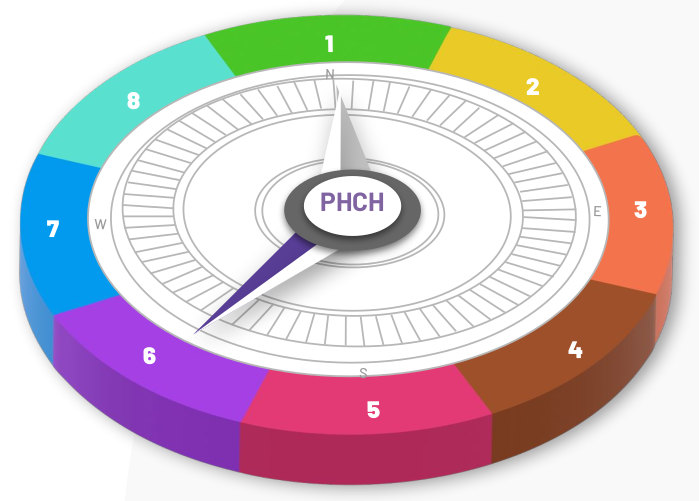
Needs of patient sub-groups are identified and systematic, pro-active approaches to deliver tailored individual planned patient care are built.
- Patients for Proactive Panel Management are identified
- Care delivery processes are redesigned
- Evidence-based decision supports are integrated
- EMRs are optimized for common clinical workflow
- Care planning processes are activated
- Team work for panel management is optimized
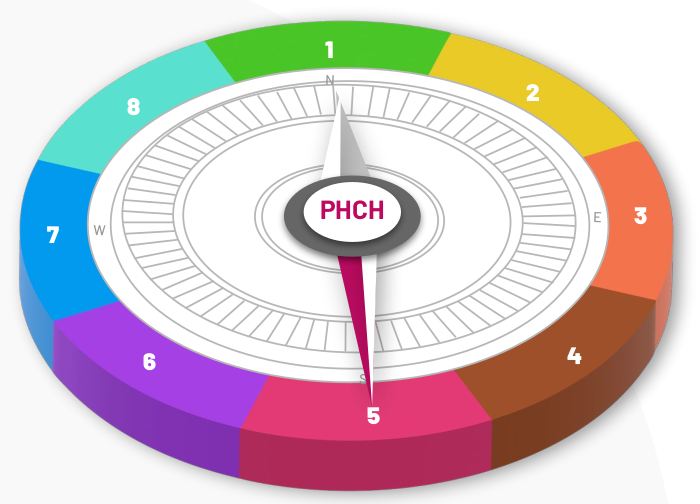
Processes designed to optimize access to appointments and to increase relational, informational and management continuity are employed.
- Supply and demand are balanced to meet panel needs without waiting
- Supply time is increased to provide care
- Panel demands for appointments are reduced
- Panels are adjusted between most responsible providers, as needed
Each patient has a dedicated primary care provider (a physician or nurse practitioner) supported by a team familiar with their story. Clinic teams coordinate screening, prevention, management and treatment needs in partnership with the patient.
- Commitments to primary care provider access and continuity are made
- Panel lists are identified and maintained
- Panel workloads are evaluated and understood
- Needs of the panels are assessed
- Patients are engaged in the improvement process
- Teams are optimized to best meet panel needs
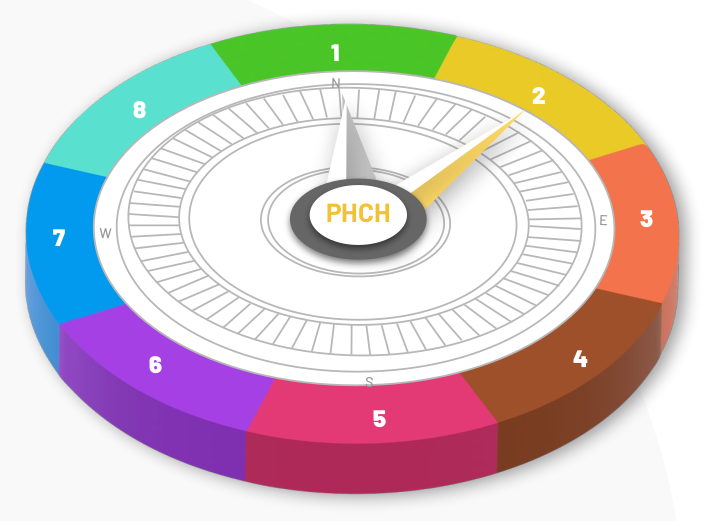
Clinic leaders and team members champion continuous improvements using proven methods.
- Clinic leaders assess and build readiness and will for change
- Quality plans are built based on the Sequence to Achieve Change
- Practice facilitation supports are identified / enhanced
- EMRs are optimized for quality improvement
- Patients are engaged in the improvement process